The Alarming Truth About Inflammation, Stress, and Autoimmune Disorders

By: Emily Brown, MS, CNS
Categories:
The Alarming Truth About Inflammation, Stress, and Autoimmune Disorders
Clients will often use the word inflammation to describe a general state of malaise, disease or dysfunction. From healthcare practitioners to dinner with friends, everyone’s talking about bodies being inflamed. But what exactly is inflammation?

Inflammation can be defined as a natural healthy reaction of the immune system as it responds to injury or infection due to a virus or bacteria and psychologically via flight, fight, or fright scenarios.
The five classic signs of inflammation include pain, heat, redness, swelling, and impaired or loss of function. For instance, when you cut your finger, the blood vessels near the wound swell and become red and irritated — this is inflammation at work, or rather, it is your immune system taking action to repair the site of injury.
Indeed, inflammation is a protective function of the immune system. When it comes to an irritant or harmful substance such as a food allergen, bacteria, virus, or stressor, the immune system attempts to remove what caused harm in the body and begin the healing process, restoring structure and function.
In the case of a cut or virus, this process involving the immune system is usually short-lived. Once the repairs are complete, the body’s immune system returns to its normal defense state.
On the other hand, inflammatory responses can become chronic, prolonged and unresolved. When the immune system mounts an inflammatory response for too long, even when there is no immediate threat or danger, health problems arise. Chronic inflammation can predispose someone to many conditions, such as heart disease, diabetes, arthritis, cancer, Alzheimer’s, depression, anxiety disorders, and autoimmune diseases.
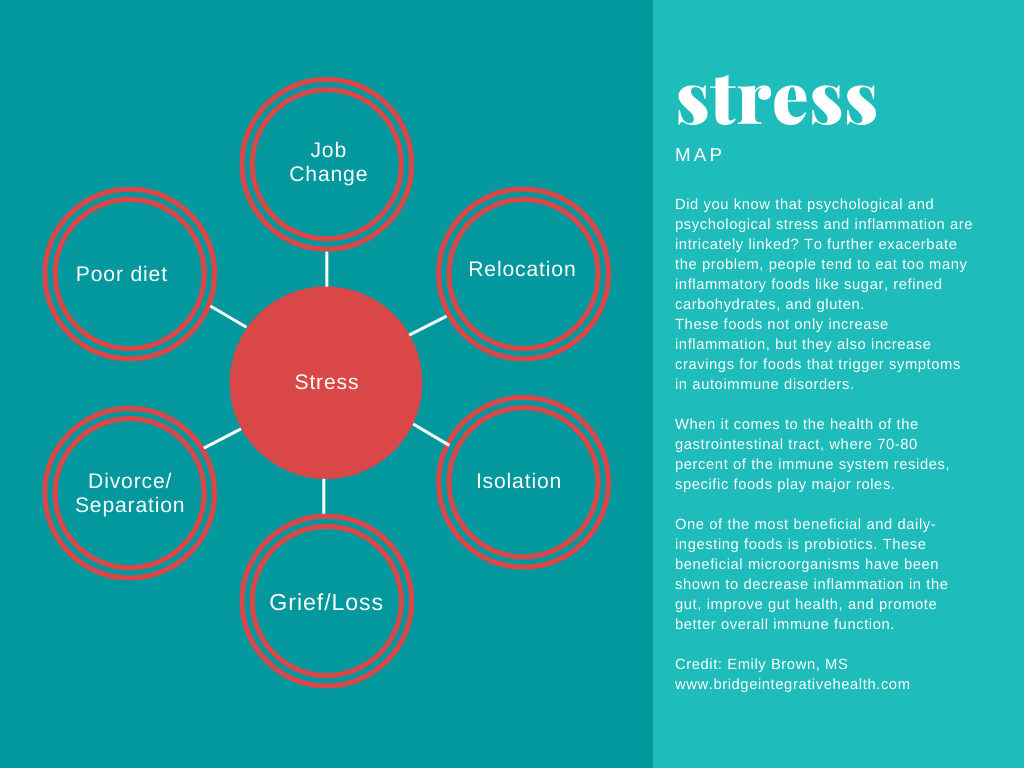
The HPA Axis and Stress
Research is clear that unresolved stress on the body is one of the worst promoters of early aging and chronic disease, and this is in large part to the inflammation that arises when one is enduring hardship of any kind. In fact, stress of all sorts causes a cascade of events that leads to premature cellular senescence (the loss of cells) in many organs. And this process accelerates as we age. The result: We get sicker faster than ever before.
The unresolved state of stress, whether emotional, physical, or perceived — or from infection or injury — triggers the immune system to respond with more inflammatory cytokines, which are proteins or cell-signaling molecules produced by the immune system.
Physiological and psychological stress also triggers the hormonal system involving the hypothalamus, pituitary, and adrenal glands, which are commonly referred to as the HPA axis. In the event of a stress-induced activity, the adrenals produce the stress hormone, cortisol. While cortisol is essential for human life, too much or too little can make day-to-day living intolerable as individuals with cortisol deficiency are plagued with fatigue and anxiety or irritability and weight gain as in the case with high cortisol.
The analogy that is best used to describe unrelenting stress is getting ready for fight or flight, with nowhere to run or staying on the run. In both cases, the body’s immune system stays on alert.
Imagine being in the woods, defenseless, when a bear begins to charge at you. You are frightened (naturally) so you begin to run (the flight response). Another possible scenario is getting attacked by a wild animal with no where to run. In this case, the fight mechanism might kick in.
In either case, when you reach a safe place, you come back to rest and this is when the HPA axis and immune system restores to balance. Yet, that recovery process can’t happen when ongoing stress is unrelenting. Whether the chronic stress is coming from a relational challenge, an unresolved infection in the body, or regularly consuming foods that might trigger an immune response, persistent stress is damaging as the body becomes exhausted trying to restore homeostasis (the normal physiological condition) and can no longer keep up.
Solutions for resolving chronic stress
Therefore, it is imperative to resolve any stress in the body, whether that stress is psychological, emotional, or physical. This includes acknowledging the effects of trauma from past experiences and current life stressors. It also means addressing self-care to boost overall health and wellbeing while living with an autoimmune disorder.
As for nutrition, increased stress and anxiety requires additional nutrients, such as B vitamins, vitamin C, minerals, vitamin D, essential fatty acids, and amino acids for neurotransmitter support. During times of duress, the cells use up any remaining stores, making it essential to take in nutrients from high-quality foods and avoiding foods that might deplete the body of essential vitamins and minerals even further.
Lifestyle factors to manage stress, such as exercise and meditation, are also important.
Here are just a few ways in which my clients, while working with me, have reduced stress in their lives:
- Removing allergenic foods and taking a quality multivitamin
- Setting boundaries in relationships at work and at home
- Establishing a sleep routine by going to bed at the same time and getting adequate sleep
- Getting regular massage therapy and other types of therapeutic modalities
- Engaging in mindfulness, meditation and prayer
- Joining a support group
- Journaling and psychotherapy
- Volunteerism and advocacy for a worthy cause
- Limiting or avoiding social media and distressing news media
- Spending time in nature, also known as forest therapy
What are your favorite ways to manage stress?
